This one is for the dedicated
-- those who study hard and work smart under pressure during emergencies
for better patient outcomes. They are Emergency Department Nurses
and Physicians; First Responders; basic, intermediate, or paramedic
EMTs; and Fire Engine and Ladder Company personnel, many of whom are
CrossFitters.
- Causes of PSVT
- Wolff-Parkinson-White
Syndrome
- An Overview of Mechanism
- Step-By-Step
- Observable Characteristics
- Vagal Maneuvers
- Potentially Lethal
- Sarah’s Story
- Summary
- Special Notes for
EMT and ER Personnel—ECG Recognition
As
its long name accurately indicates, paroxysmal supraventricular tachycardia
(PSVT) is a rapid heart rate that begins and ends abruptly, unlike normal
and functional sinus tachycardia, which begins and ends gradually.
It is called “supra-ventricular” because the focus is not in the
ventricles and the ventricular complexes on the ECG are normal (narrow).
Please refer to last month’s article (“Functional Exercise-induced
Tachycardia”) for more information on sinus tachycardia.
CAUSES
There
are two main causes of PSVT, AV nodal reentry (50%) and circus (circular)
movement tachycardia (40%), sometimes called “AV reentry”.
AV nodal reentry tachycardia (AVNRT) is usually benign and can be terminated
with a vagal maneuver, although sometimes it requires more aggressive
treatment..
Circus
movement tachycardia (CMT) is seen in individuals with Wolff-Parkinson-White
(WPW) syndrome and is potentially lethal because of the unexpected
abnormal heart rhythms that can occur due to its anatomical substrate.
Those arrhythmias are the subject of this article.
WOLFF-PARKINSON-WHITE (WPW)
SYNDROME
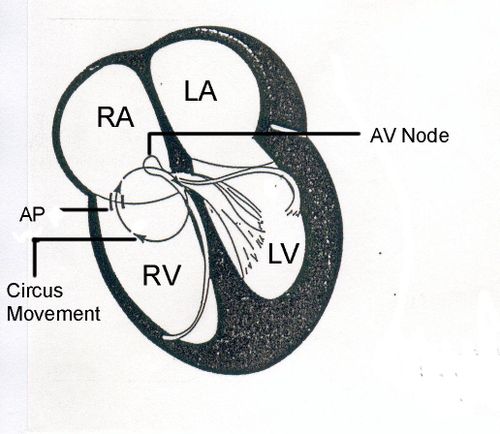
In
WPW syndrome, there is an extra microscopic strand of muscle fibers,
called an “accessory pathway” (AP), connecting an atrium to a ventricle.
All muscle fibers conduct current rapidly---more rapidly than the atrioventricular
(AV) node, the normal connection between the atria and the ventricles.
During
normal sinus rhythm, the impulse may enter the ventricles slightly early
using the rapidly conducting AP (Fig. 1), which usually leaves a sign
of early ventricular activation on the ECG known as a delta wave.
The
size of the delta wave can be anywhere from very tiny to very big when both ventricles are captured by the delta force, depending upon
how soon that current arrives in the ventricle prior to activation across
the AV node, its normal route.
In
Fig. 1 the sequence of activation is indicated. Note that even
though the journey from the sinus node to the accessory pathway is longer
than from the sinus node to the AV node, AP conduction is swift, producing
a medium sized delta wave on the ECG. The delta wave is of course not
a danger of itself. But, as you will see, the AP can cause big
trouble when blocked.
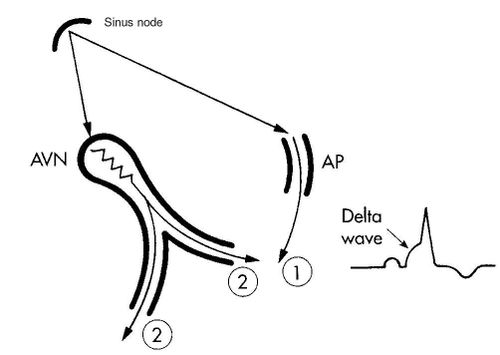
Fig. 1. A diagrammatic
representation of early activation of the left ventricle across an AP
(1). The activation of the ventricles across the AVN (2) is a little
slower.
AP = accessory pathway; AVN
= atrioventricular node
- A normal sinus impulse
(top) is shown penetrating the accessory pathway first, leaving no possibility
for retrograde penetration from the ventricles once they are activated.
The early activation of the ventricle is reflected by a delta wave on
the ECG. Circus movement tachycardia does not develop in this
milieu.
- There is delay crossing
the AV node so that activation of the ventricles across this normal
pathway lags slightly behind the abnormal penetration.
It is also possible for
the delta wave to be absent because of a latent or concealed AP.
With the latent type, even with a normal ECG, the contribution of an
accessory pathway in the production of PSVT or atrial fibrillation is
still possible. The diagnosis is suspected by a well-informed examiner
because of a history of PSVT and confirmed with electrophysiological
testing.
The
term favored by many Electrophysiologists and Cardiologists for Wolff-Parkinson-White
Syndrome is “Preexcitation Syndrome”---although not easily abbreviated,
it is a far more accurate designation, with all due respect to Drs.
Wolff, Parkinson, and White, who believed in 1930 that they were looking
at bundle branch block---not the same1.
AN OVERVIEW OF MECHANISM
Circus
movement tachycardia uses two pathways to complete a circle of excitation
between the atria and the ventricles. In Fig. 2, the circuit is
shown moving up the AP to the right atrium (RA) and down the AV node
into the ventricles.
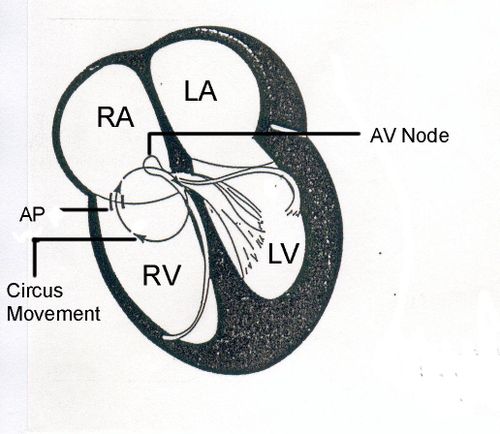
Fig. 2. A diagrammatic
representation of the mechanism of circus movement tachycardia using
a right-sided AP in the retrograde direction.
AP = accessory pathway; AV
= atrioventricular
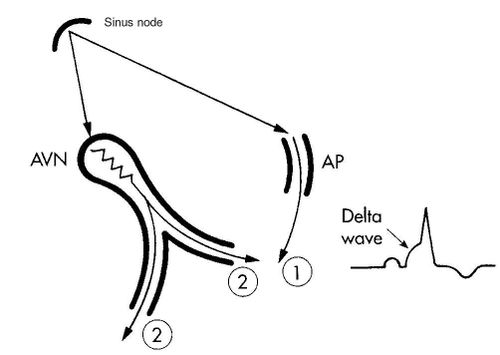
STEP-BY-STEP
The Beginning of Circus
Movement Tachycardia

Fig. 3.
Circus movement
tachycardia usually begins with one errant (ectopic) atrial beat, indicated
by the asterisk. The 1-2-3 events that follow are as indicated
-- sequential.
- The early atrial
beat (*) is blocked in a left-sided accessory pathway (AP).
- The excitation wave
enters the ventricles normally across the AV node.
- The AP still has
not been activated and is an open channel for retrograde penetration
from the ventricles, setting the stage for a reentry circuit and PSVT.
Note the reentry of the impulse into the atria at number 3.
Continue with Fig. 4 to
see the next sequence when the impulse has dashed up the open AP and
whips around to activate the AVN and start around again.
The Maintenance of Circus
Movement Tachycardia

Fig. 4.
Around and around the current goes in this sequence:
Atria↑AV node↑ventricles↑accessory pathway↑
Atria↑AV node↑ventricles↑accessory pathway↑
etc etc etc --- PSVT!
A reentry circuit thus established,
continues until its path is interrupted, usually when a vagal maneuver
slows or blocks conduction in the AV node.
In Fig. 4, draw an imaginary line across the AV node (AVN) where you see
conduction slowing. This is what happens with a vagal maneuver---the
circuit is interrupted and the sinus node will pick up its cadence
once again---slowly at first because it has been suppressed.
OBSERVABLE CHARACTERISTICS
Heart rate. Around
200 beats/min. (range 170-250).
Heart rhythm. Begins abruptly;
maintains a regular rhythm; ends abruptly with a vagal maneuver.
Frog sign.
During PSVT
atria and ventricles are contracting simultaneously. The force
generated by the ventricular contraction pushes blood up against the
AV valves and shuts them tight. Thus, during atrial contraction the
flow of blood normally destined for the ventricles is blocked by
closed pressure-locked AV valves (mitral and tricuspid) and has
nowhere to go but the wrong way--up. This causes a reflux up the
jugular neck veins with every atrial contraction, causing the
jugulars to bulge in time with the atrial contraction---fast and
regular, like the regular puffing seen in a frog. Obesity precludes
visibility of the jugular veins.
It is important to understand that
these pulsations in the jugular veins are regular in PSVT. Try vagal
maneuvers; if that doesn’t work, call 911.If the
heart rate is rapid and there are only occasional pulsations or no
pulsations at all in the jugular vein, call 911 and have the AED
ready.
VAGAL MANEUVERS
A vagal maneuver
blocks the AV node, which is a critical choke point in the circuit just
described. Vagal maneuvers create pressure in the pressor receptors
(baroreceptors) located in several places in the body, but mainly in
the aortic arch and carotid sinus. Sensing too much pressure,
the message is sent to the brain, stimulating the vagus nerve.
The effect is to slow conduction velocity in the AV node and interrupt
the circuit, thus terminating the tachycardia. Some prehospital vagal
maneuvers are:
- Coughing (deeply)
- Straining
- Lying on the floor
with legs elevated against the wall
- Blowing against
a closed glottis
- Gagging (finger
down the throat type)
- Rising from a deep squat
If one doesn’t
work, try another. Some people will not respond to the deep cough,
but will convert to normal rhythm immediately when their legs are propped
straight up. In the hospital setting, the physician will use carotid
sinus massage, and for the very young, immersion of the face in cold
water (the dive reflex). If the vagal maneuver stops the
tachycardia, the person will usually feel OK and can carry on.
However, they must see a Cardiologist and be cleared of any suspicion
of overt or latent WPW syndrome.
POTENTIALLY LETHAL
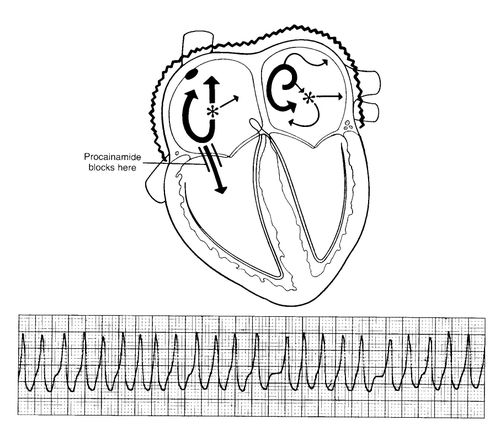
Atrial
fibrillation. PSVT may result in atrial fibrillation, in which
case many erratic electrical currents are causing the atria to quiver
(fibrillate). When there is an accessory pathway offering a very
rapid detour into the ventricles, the ventricular rate will be irregular
and 200-300 beats/min. Atrial fibrillation can be lethal if it
converts to ventricular fibrillation. .
When
the atria are fibrillating and WPW syndrome is not present, the rate
of the ventricles is controlled by a prescription medication.
Thus, of itself, atrial fibrillation is not life threatening.
It is a different story when there is an accessory pathway for rapid
entry from an atrium into a ventricle---THAT is life threatening.
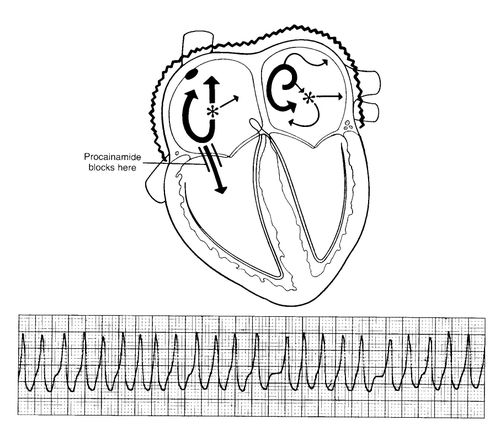
Fig. 5. Atrial
Fibrillation in a Patient with Wolff-Parkinson-White Syndrome.
In the atria there are multiple electrical currents, many of which pass
rapidly down the accessory pathway to activate the ventricles.
Even
if one has never seen an ECG tracing before, the rapid (210 beats/min)
irregular spikes in Fig. 5 would be alarming. Not all of these
beats are felt at the peripheral pulse because the ventricles are not
filling completely during each cycle.
In
spite of such a rapid heart rate and a reduced cardiac output, there
are cases where a young, fit person with this arrhythmia drives to and
walks into the ER. Having done so, the danger is that this rhythm
will not be diagnosed soon enough or even correctly, and thus degenerate
into ventricular fibrillation.
Ominous physical signs
of conversion to atrial fibrillation.
NOTE: 911 should
already have been called and the AED made ready.
There are three visible signs
of conversion from PSVT to atrial fibrillation in cases of WPW syndrome.
- The
“frog sign” disappears---every time.
- The hemodynamic
condition worsens, i.e. the person may become unconscious, but this
is not always the case.
- The heart rhythm
is irregular, although at such rapid rates this may be impossible to
appreciate without an ECG recording.
SARAH’S STORY
Sarah
Kerlin is a national cyclocross champion, international competitor,
trusting believer, and very lucky survivor who happened to be in the
right locker room at the right time.
For
a chapter on “The Athlete’s ECG”, I wanted original ECGs from
some of the top athletes in our Santa Cruz community. Among them
was Sarah, who graciously allowed me to record her. My expectation
was to see ECG evidence of an elite athlete, nothing more. What
showed up was much more--Wolff-Parkinson-White (WPW) syndrome, which,
upon questioning her, turned out to be dangerously symptomatic and life
threatening. When asked if she had ever felt a sudden acceleration
of her heart rate; her answer was a resounding and surprised-to-be-asked:
“YES, every morning when I wake up and once during competition.”
Alarm bells!! She had no idea of the danger she was in.
After
that we moved quickly and urgently. Finally, one morning I drove
her into UCSF for her appointment with Dr. Mel Scheinman, Director of
Cardiology. Dr. Scheinman and his experienced crew of physicians
threaded a catheter into Sarah’s heart, identified the accessory pathway,
and delivered radiofrequency energy to heat up and destroy that tiny
errant strand of conductive muscle connecting her atria to a ventricle.
Just like that—diagnosed on the locker room floor and cured two weeks
later with an eloquent procedure in expert hands! Her alarming rapid
heart rate wake-up call is now a faded memory. Sarah never doubted—just
went ahead with what had to be done.
SUMMARY
- Remember that sinus
tachycardia is normal when physically active, frightened, or otherwise
emotionally involved. It starts gradually and returns to normal
gradually --- nothing sudden. Please review “Functional Exercise-Induced
Tachycardia” Aug’09.
- Paroxysmal supraventricular
tachycardia (PSVT) begins and ends abruptly.
- The diagnosis of
PSVT can be made without an ECG because of the frog sign--a regular
pulsing in the neck (jugular) veins similar to a puffing frog. However,
the differential diagnosis between circus movement tachycardia and AV
nodal reentry tachycardia is only made with multiple ECG leads.
- Remember that the
regularity of the pulsing in the jugular veins is significant. Fast
and regular = PSVT. If there is no pulsing or irregular slow pulsing
in the jugulars, call 911, stay with the victim, and have the AED ready.
- PSVT can usually
be stopped by a vagal maneuver.
- Atrial fibrillation
in a person with an accessory pathway is potentially fatal.
Call 911; have the AED ready. There is no frog sign
in the neck veins. Vagal maneuvers do not help. There is a pulse,
but it is very fast and irregular.
- If there is no pulse,
defibrillate immediately. If no AED, start CCR. (see “What Happened
to CPR”)
SPECIAL NOTES FOR EMTs AND
ER PERSONNEL---ECG RECOGNITION
If the patient
is conscious, do not terminate the tachycardia before you record it.
The ECG is your only shot at a differential diagnosis for this patient,
possibly after many symptomatic years of undocumented bouts with PSVT.
- Quickly record a
12 lead ECG or at least I, II, III, and V1
- Check for P location,
P axis, QRS alternans, and aberrant ventricular conduction---all are
helpful in the differential diagnosis and are explained briefly below.2,
3
- Jugular pulse: Frog
sign = AVNRT or CMT; flutter waves = atrial flutter; irregular cannon
A waves = VT.
- Try a vagal maneuver,
which is diagnostic if it is atrial flutter (saw-tooth pattern seen);
if it is PSVT it’s therapeutic (stops the tachycardia.).
- If that doesn’t
work, follow your drug protocol, e.g.: adenosine, if that doesn’t
work—procainamide—if that doesn’t work--cardiovert. 2
- Record the sinus
rhythm in the same leads for comparison (helps find Ps).
P location.
In AVNRT the P distorts the end of the QRS (psuedo r in V1
or psuedo s in inferior leads) or is completely hidden within the QRS
In CMT the
P wave is always separate and usually closely follows the QRS
(RP<PR). Whether you see a delta wave in the sinus rhythm tracings
or not---this patient has an accessory pathway and should be admitted
for evaluation for RF ablation.
P axis.
Positive P waves in II, III, aVF indicate atrial tachycardia and rules
out CMT and AVNRT. Negative P waves in II, II, aVF indicate AVNRT
or CMT using a posterior septal AP. These are possibly the most
useful ones.
QRS alternans
(alternating heights of R peaks or depth of S nadirs) is a common occurrence
(25-30% of the time) in CMT. Look for it first, examining all
leads carefully. It is very uncommon to find this clue in AVNRT
after the first few minutes.
Aberrant
ventricular conduction. Aberrancy is more common in CMT than it
is during AVNRT and is therefore helpful in the differential diagnosis.
Jugular
pulse. Frog sign (fast regular expansion) = PSVT. Flutter
waves = atrial flutter. Occasional cannon A waves during tachycardia
= AV dissociation and is diagnostic for VT.
ATRIAL FIBRILLATION IN WPW
SYNDROME
- ECG: Fast, Broad,
Irregular (FBI) Looks like VT except it is irregular; VT is usually
regular. Fast because of rapidly occurring atrial
impulses using a rapidly conducting AP; Broad because of
ventricular activation outside the conduction system; Irregular
because of atrial fibrillation and concealed conduction into the AV
node and AP.
- If hemodynamically
unstable, cardiovert.
- Do not use verapamil
(danger of severe hemodynamic deterioration).
- Use procainamide.
It prolongs the refractory period of the AP, the ventricles, and the
retrograde fast AV nodal pathway. It may therefore slow conduction across
the AP and the ventricular rate during atrial fibrillation. It
may also terminate VT, CMT, and the common form of AVNRT.2,
3
- If procainamide
doesn’t slow the ventricular rate, cardiovert.
ACKNOWLEDGEMENTS
Hein J.J. Wellens M.D.,
Professor of Cardiology at the University of Maastricht in the Netherlands
and formerly Chairman of the Department of Cardiology at University
Hospital, Maastricht approved the section for ER personnel and EMTs.
I would like to thank him for his continued support and encouragement.
Heather
MacDougall’s (CFSC) review and
comments prompted me to add the step-by-step illustrations.
Skip Hanson (CFSCC)
was encouraging with his review of the manuscript in its developmental
stages.
The artwork is that of Rene’
Fontan, West Hills, California.
Elsevier Publishing Co.
holds the copyright on the illustrations.
REFERENCES
1. Wolff L, Parkinson J, White
P, et al: Bundle-branch block with short P-R interval in healthy young
people prone to paroxysmal tachycardia, Am Heart J 5:685, 1930.
2. Wellens HJJ, Conover M:
The ECG in emergency decision making, 2ed, Elsevier, 2006, St. Louis.
pp 107 and 153.
3. Conover MB: Understanding
electrocardiography, 8ed, Elsevier, 2003, St. Louis. pp. 275-300.



 Sunday getting filthy
Sunday getting filthy
 Having fun.
Having fun.
 Chris running backwards
Chris running backwards
 Last year at the open.
Last year at the open. Cal Fire Crew
Cal Fire Crew
 Coach D
Coach D Duffy and Chris playing horse.
Duffy and Chris playing horse.


